Most enterprise health‑care buyers are asking tougher security questions than ever. Procurement teams want proof that your organisation limits what it collects and shares; regulators look at whether personal health data is truly needed for each use; and attackers know that sprawling data stores are prime targets. In this HIPAA Data Minimization Guide, I draw on more than 25 years of combined experience and over 6,000 audits delivered through Konfirmity to show why minimisation isn’t a buzzword but a concrete set of practices. You’ll see how the minimum necessary rule protects protected health information (PHI), how strong data governance supports sales and compliance, and how to put these principles to work in real systems. Expect practical insights rather than generalities. The aim is to equip CTOs, CISOs and compliance leaders with a map for collecting only what you need, curbing who can see it and disposing of what you no longer require.
Why Data Minimisation Matters Under HIPAA
HIPAA’s Privacy Rule is built on a simple idea: patient data shouldn’t be used or shared when it isn’t needed. The minimum necessary standard requires covered entities to evaluate their practices and limit unnecessary or inappropriate access to PHI. This isn’t just regulatory fine print. Reducing the quantity of PHI you hold and share lowers the impact of a breach and improves resilience and trust. IBM’s 2025 Cost of a Data Breach Report reports U.S. breaches averaging $10.22 million and health‑care breaches averaging $7.42 million, and that health‑care breaches take an average of 279 days to identify and contain. These figures show why narrowing your attack surface is critical: fewer records mean fewer endpoints to defend and faster investigations.
Data minimisation also supports efficient operations. Collecting only what you need means fewer records to maintain, fewer systems to secure and less time spent on access reviews. We routinely see health‑care vendors cut their SOC 2 or ISO 27001 readiness timeline from nine to twelve months down to four to five months when they adopt a purpose‑driven data strategy and rely on managed services. In one tele‑health engagement, clarifying retention schedules and rightsized access cut annual audit preparation from hundreds of hours to about 75. The result: teams focus on care delivery while controls stay evidence‑ready.
Regulators pay attention. Since 2003, the Office for Civil Rights (OCR) has resolved more than 374,000 HIPAA complaints and conducted over 1,193 compliance reviews. OCR settlements and civil money penalties have exceeded $144 million, and the most common issues include impermissible uses and disclosures, lack of safeguards, denial of patient access and failure to limit the information disclosed. One of the frequent findings is using or disclosing more than the minimum necessary. These numbers show that enforcement is real and that minimisation failures are costly.

What Is Data Minimisation Under HIPAA?
Data minimisation means collecting, using and disclosing only the personal health information necessary for a defined purpose and retaining it only as long as needed. It originates from privacy principles common in national and international frameworks. NIST calls the practice of limiting the use, collection and retention of personally identifiable information a basic privacy principle. Limiting PHI collections to the least amount necessary “may limit potential negative consequences in the event of a data breach”. HIPAA expresses the same idea through its minimum necessary standard and through the broader requirement to safeguard PHI using administrative, physical and technical controls.
Under HIPAA, data minimisation is not optional. The Privacy Rule requires covered entities to take reasonable steps to limit uses and disclosures of PHI to the minimum necessary to accomplish the intended purpose. Internal policies must identify who needs access to information to carry out their duties, the categories of PHI needed and any conditions attached to that access. This ensures that everyone—from clinicians to billing clerks—only sees what they need. Minimisation ties directly to patient confidentiality and risk reduction: the fewer systems and people that handle sensitive data, the lower the chances of accidental disclosure or malicious access.
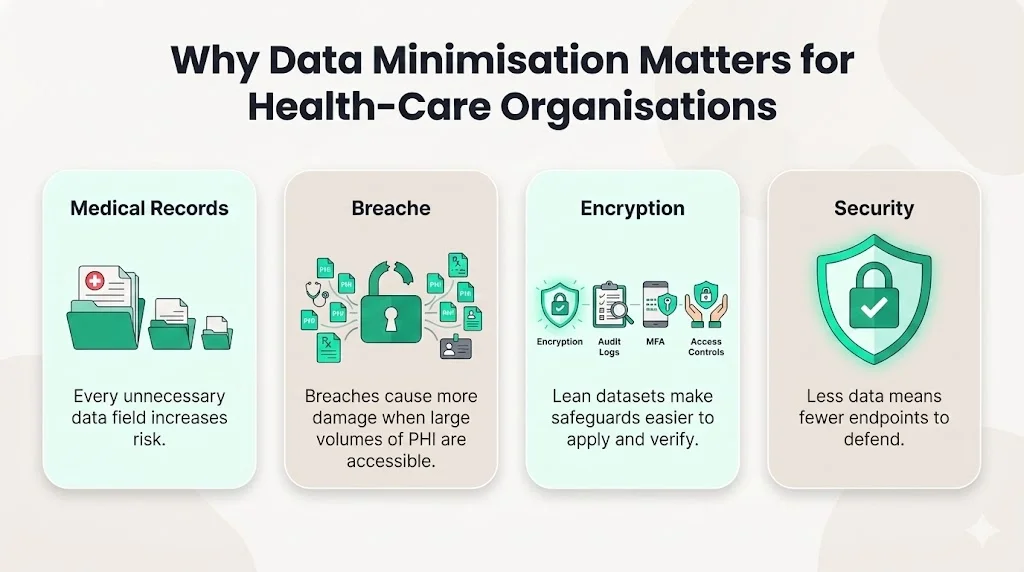
Why Data Minimisation Matters for Health‑Care Organisations
Minimising the data you collect and store drives down risk and enhances security. Every unnecessary field expands your attack surface. Breaches often begin with compromised credentials, but they become more damaging when attackers can roam across large troves of PHI. The HIPAA Security Rule states that access controls should let authorised users view only the information needed for their job functions. When you hold less data up front, you have fewer endpoints to defend, fewer logs to review, and less to encrypt. Encryption, audit logging and integrity checks are core technical safeguards; a proposed update to the Security Rule would make encryption and multi‑factor authentication mandatory. These protections are easier to implement and verify when the dataset is lean.
Data minimisation also streamlines audits and supports access control policies. Auditors ask how organisations map PHI, why they collect it and who can see it. When each data element has a clear purpose and lifecycle, those answers are straightforward. Over the course of 6,000+ audits, we’ve seen that companies with disciplined inventories and retention schedules have fewer findings and shorter audit timelines. By limiting PHI to well‑defined systems and roles you can cut your audit preparation time by up to 40 percent and avoid corrective actions like those levied against entities that fail to assess risks. Strong access control policies—which the technical safeguards paper requires—are simpler to enforce when each role is mapped to only the fields necessary for that role. Minimisation therefore reinforces least‑privilege and reduces privilege creep.
HIPAA Minimum Necessary Standard Explained
The HIPAA Data Minimization Guide emphasises that understanding the minimum necessary standard is central to applying minimisation in practice.
Core Rule Elements
The minimum necessary standard in 45 C.F.R. § 164.502(b) and § 164.514(d) requires covered entities to limit uses, disclosures and requests for PHI to what is needed for the intended purpose. Entities may rely on standard protocols for routine disclosures, such as eligibility checks, but must review non‑routine disclosures case by case. Organisations should identify which workforce classes need access, what categories of PHI they require and any conditions for access. The rule allows flexibility; entities must define “necessary” based on their workflows and document their decisions.
Exceptions
The rule has specific exceptions: disclosures for treatment, disclosures to the individual, uses authorised by the patient, compliance with other HIPAA rules, enforcement requests from HHS and uses required by law. For billing, quality improvement, marketing or research without authorisation, the minimum necessary standard still applies.
Applicability
Covered entities include health plans, health‑care clearinghouses and providers that transmit certain transactions electronically. Business associates—vendors that create, receive, maintain or transmit PHI on behalf of a covered entity—must also follow the standard through their contracts. Startups often discover this obligation only when a buyer requests a business associate agreement (BAA); signing a BAA means having minimum necessary policies, controls and documentation ready.
How the Standard Protects PHI
The minimum necessary principle reflects a core security concept: not all data is needed for every use case. Limiting the scope of data used and disclosed reduces the probability and impact of wrongful access. HHS notes that covered entities should implement policies that identify which workforce members need access, what types of PHI they need and under what conditions. Access controls should enable authorised users to view only the minimum information necessary for their roles. This approach strengthens patient confidentiality by preventing unnecessary exposure of diagnosis codes, financial details or identifiers during administrative tasks. When combined with technical safeguards like encryption and audit logging, the minimum necessary standard creates multiple layers of defence against insider misuse and external attacks.
Core Principles of Data Minimisation
Our HIPAA Data Minimization Guide distils minimisation into four core principles that drive day‑to‑day decisions about collecting and handling PHI.
- Purpose‑Driven Collection. Before collecting any PHI, articulate why you need it and collect only what is essential. Remove fields that do not serve a clinical, billing or regulatory need.
- Scoped Access. Grant access based on job duties and review rights regularly. Implement unique user IDs, session logoff and multi‑factor authentication to ensure only authorised users can view PHI.
- Regular Evaluation and Data Lifecycle Management. Regularly review whether existing data is still needed and destroy records that no longer serve a purpose. Use retention schedules and automated purges to enforce this lifecycle.
- Encryption and Safeguards. Use strong encryption to convert data into unreadable text. Complement this with audit controls, integrity checks and authentication procedures to ensure even the limited data you hold is protected.
Applying Data Minimisation Across Your Organisation
This part of the HIPAA Data Minimization Guide shows how to translate principles into actions across data collection, access control and disclosures.
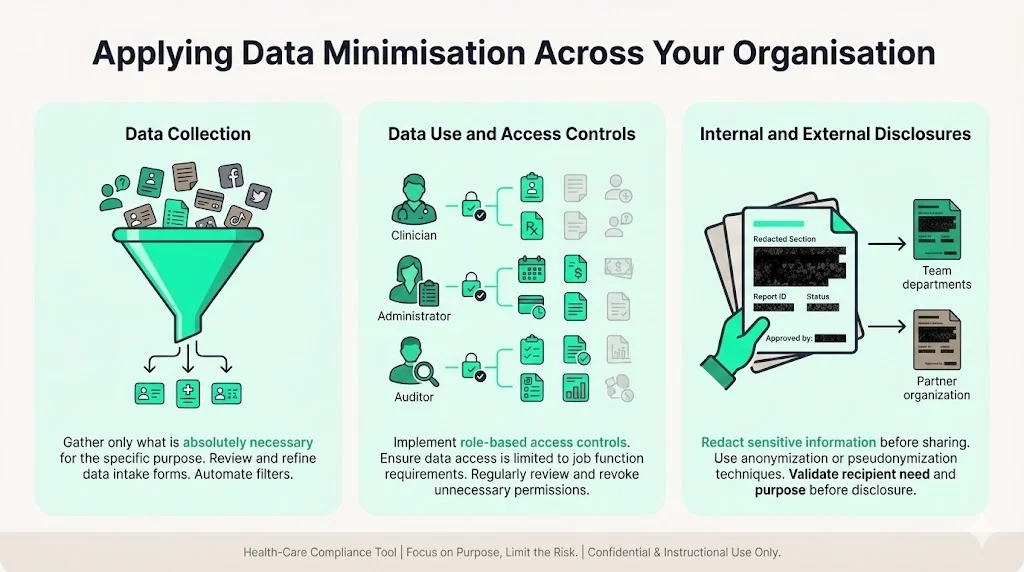
Data Collection
Set clear rules for what PHI you collect and why. Start with a data inventory of all systems where PHI enters your environment. For each field, define its purpose and lawful basis, and remove optional fields that are not essential. Match these decisions to security policies and regulatory requirements. A lean intake reduces storage costs, security obligations and simplifies consent and deletion under overlapping frameworks like the GDPR.
Data Use and Access Controls
Role‑based access is essential. Build matrices that map job titles to specific PHI fields and enforce them through system roles. Use group membership and attribute‑based policies to automate provisioning. The minimum necessary standard encourages covered entities to identify which persons need access and to limit it accordingly. Review privileges regularly to detect creep. Record who accesses what and when and feed these logs into monitoring systems. Making logging automatic reduces the burden of evidence collection during audits.
Internal and External Disclosures
When sharing PHI internally or externally, apply the same minimisation logic. Clinicians may need full records, but administrative staff often need only demographic or billing data. For external disclosures—such as research or insurance—use agreements that specify the purpose, authorised fields and retention obligations. The minimum necessary standard exempts disclosures for treatment and patient access, but other disclosures require case‑by‑case review. Use a review process to verify that the disclosure meets these rules and that the recipient has adequate safeguards.
Tools and Techniques to Support Minimisation
Technical and Administrative Safeguards
Several technical safeguards underpin the HIPAA Data Minimization Guide. Encrypt electronic PHI at rest and in transit so that data becomes unreadable without a cryptographic secret; a proposed rule would make encryption and multi‑factor authentication mandatory. Record who accesses what and when by implementing audit controls, and use integrity checks such as hashes or cryptographic signatures to detect improper alteration. Verify identities with unique user IDs and multi‑factor authentication. These measures work best when the dataset is small and purpose‑driven.
Administrative safeguards set the rules for data minimisation. Document why each data element is collected and how long it is retained. Conduct thorough risk analyses to identify vulnerabilities and implement measures to bring risks down to an appropriate degree. OCR settlements show that ignoring this step invites enforcement. Include vendors by requiring business associate agreements that mandate compliance with the minimum necessary standard and specify encryption, logging and retention obligations. Training should reflect your operations—HHS notes that no single programme fits all organisations. Teach staff to collect only what’s necessary, avoid over‑collection and handle non‑routine requests carefully. Use scenarios from your environment to illustrate common pitfalls, such as exporting unencrypted spreadsheets or copying PHI into collaboration tools.
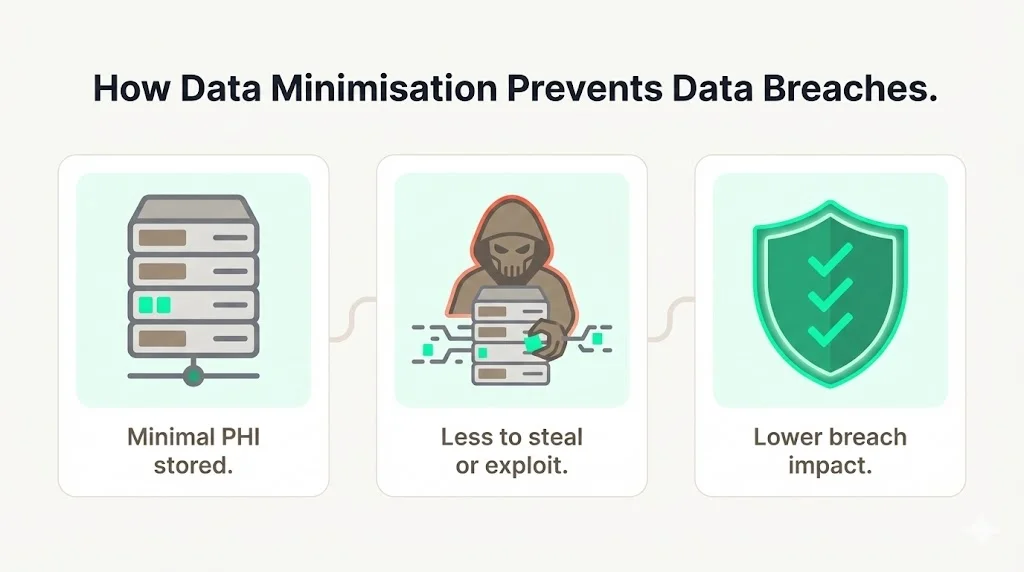
How Data Minimisation Prevents Data Breaches
Limiting the volume of PHI you hold reduces the potential impact of a breach. Attackers who gain access to a database containing minimal data have less to monetise or exploit. IBM’s report highlights that detection and escalation costs, lost business and post‑breach response make up the largest components of breach costs. Reducing stored data reduces the scale of these costs and simplifies encryption because there are fewer secrets to manage and less complexity. Coupled with multi‑factor authentication, network segmentation and regular vulnerability scanning—all of which the proposed rule would require—minimisation forms a holistic defence.
The IBM report also notes that strong encryption and security automation significantly reduce breach costs. When PHI is encrypted and minimised, lost or stolen devices have little value. Investing in minimisation and encryption can therefore yield a measurable return by reducing the cost per record. Likewise, a short data retention window lowers legal liabilities and speeds forensics. Organisations that combine minimisation with continuous monitoring and incident response planning recover faster and maintain trust during a crisis.
Monitoring and Continuous Improvement
Minimisation isn’t a one‑time project; it is a continuous discipline. Review policies and technical controls at least annually to ensure they still fit your operations and regulatory obligations. The Security Rule directs covered entities to deploy technical controls consistently and to test their effectiveness every 12 months. Use these reviews to remove stale data, revoke unneeded permissions and adjust to new threats. Invest in monitoring that flags anomalous behaviour—such as unusual database queries or repeated failed authentication—and integrate alerts with incident response. Track metrics like audit log coverage and time to revoke dormant accounts to guide improvements. As OCR issues new rules—such as mandatory encryption or multi‑factor authentication—update your policies and systems promptly so your minimisation practices remain effective.
Practical Checklist for Busy Teams
Use this condensed list to embed data minimisation into day‑to‑day operations:
- Map Where PHI Lives. Build a data inventory covering applications, databases, file stores and third‑party platforms.
- Define Purpose for Each Data Element. For every field, document why it is collected, the lawful basis and the retention period.
- Restrict Access by Role. Implement role‑based access control and enforce least‑privilege principles; use multi‑factor authentication for all administrative access.
- Encrypt PHI and Log Access. Apply strong encryption at rest and in transit; implement audit controls to record who accessed what.
- Train Staff Regularly. Provide role‑specific training on your data handling policies and on recognising when requests for PHI exceed what is necessary.
- Schedule Regular Policy Reviews. Conduct annual risk analysis and policy updates; adjust controls based on emerging threats and regulatory changes.
Conclusion
Data minimisation goes further than a compliance duty. It is a practical strategy for protecting patients and supporting the business. The minimum necessary standard requires covered entities and their partners to limit uses and disclosures of PHI to what is required. Implementing purpose‑driven collection, scoped access, regular data lifecycle reviews and strong technical safeguards reduces the risk of breaches and simplifies audits. Health‑care organisations that embed these practices see shorter sales cycles, fewer audit findings and greater resilience when incidents occur. As regulators move towards mandatory encryption, multi‑factor authentication and continuous risk assessments, adopting minimisation now positions you ahead of the curve.
Minimisation also has benefits outside HIPAA. It matches SOC 2 and ISO 27001 requirements to limit collection, implement least‑privilege and manage retention. Under the GDPR’s data minimisation principle, organisations must collect personal data only for specified purposes and store it for no longer than necessary. By defining purposes and retention windows, you can use controls and evidence across frameworks, reducing the cost and time to achieve multiple certifications. Many Konfirmity clients use one set of minimisation controls to satisfy SOC 2 Type II, ISO 27001:2022 and HIPAA simultaneously. This cross‑framework reuse accelerates due diligence with enterprise buyers and simplifies annual recertifications.
Konfirmity’s human‑led, managed security and compliance service was built on these principles. We start with security and arrive at compliance, implementing controls inside your stack and managing evidence year‑round. The result is fewer findings, faster buyer approvals and a programme that stands up under real‑world pressure. Security that reads well but fails in practice is a liability. Build your programme once, operate it every day and let compliance follow.
FAQs
Q1: What are the three main points of data minimisation?
The core points are purpose‑driven collection, scoped access and regular review. Collect only the PHI needed for the task, restrict access to authorised personnel and regularly review your holdings to remove data that no longer serves a business purpose. These principles reduce the data you must protect and limit the impact of a breach.
Q2: What are three requirements of HIPAA’s minimum necessary rule?
Covered entities must take reasonable steps to limit uses and disclosures of PHI to the minimum necessary; define the classes of persons who need access and the categories of information they require; and develop policies and procedures for routine and non‑routine disclosures. Exceptions apply for treatment purposes, disclosures to the individual, authorisations and certain legal requirements.
Q3: What is the best way to minimize incidental HIPAA violations?
Provide regular training so staff know what PHI they truly need for their tasks, implement role‑based access and multi‑factor authentication so that unauthorized individuals can’t view PHI, and maintain audit logs to detect and respond to unusual access. Clear procedures for handling non‑routine requests ensure that employees don’t release more data than necessary.
Q4: What are the main principles of data minimisation?
Purpose limitation—collect data for specific purposes only—and data volume limitation—collect only what’s needed—are foundational. Access limitation follows: give access only to those who require it. Finally, regularly review and dispose of data that is no longer required. Together these principles reduce risk and support compliance.





.svg)






.svg)
.svg)