Most enterprise healthcare buyers now demand proof that security programmes work. When electronic protected health information (ePHI) is at risk, deals stall and regulators impose larger penalties. HIPAA Data Residency sits at the centre of this scrutiny. It answers three questions: where does sensitive health data live, how is it secured, and under what laws does it fall? This article demystifies HIPAA’s requirements, explains why data location matters in 2026 and outlines practical steps drawn from more than 6,000 audits.
HIPAA’s requirements and data location
The Health Insurance Portability and Accountability Act is designed to protect patient privacy and ensure that ePHI is kept secure. Its Privacy Rule defines how information may be used and disclosed, while the Security Rule requires covered entities and business associates to ensure the confidentiality, integrity and availability of ePHI. Those rules expect organisations to conduct a thorough risk analysis to identify threats and vulnerabilities and then implement appropriate safeguards. HHS’ guidance notes that risk analysis and risk management are foundational to compliance and that the Security Rule allows flexibility of approach. Risk management must reduce risks to a reasonable and appropriate level.
HIPAA does not prescribe a storage country
Many teams interpret HIPAA as a residence law and assume that storing data in a particular state or country guarantees compliance. That is a misconception. The law does not mandate a specific geographic location for storing ePHI. The HIPAATimes points out that HIPAA does not explicitly require data localisation within United States borders. Instead it demands that organisations implement administrative, technical and physical safeguards, maintain audit controls and sign business associate agreements (BAAs) when sharing data. Paubox’s guidance echoes this: compliance depends on the provider’s security measures, encryption, access controls and willingness to sign a BAA, regardless of where servers are located.
What HIPAA does require
Even though there is no location mandate, HIPAA sets clear expectations for how data is protected:
- Risk analysis and risk management – Entities must identify where ePHI is stored, used or transmitted and assess potential threats. HHS emphasises that risk analysis and management are fundamental to security.
- Access controls, audit trails and authentication – The Security Rule mandates procedures to limit who can view or modify ePHI and to monitor these actions. Encryption is an addressable safeguard, meaning organisations must decide whether and how to encrypt and document the decision.
- Transmission security – ePHI moving between systems must be protected against interception. Entities must determine appropriate encryption and integrity controls and document these choices.
- Business associate agreements – Every vendor that stores or processes ePHI must sign a BAA that specifies roles, responsibilities and incident reporting.

Why location still matters
The absence of an explicit residency mandate does not make location irrelevant. Where data lives affects legal jurisdiction, access control and risk. Data stored in a cloud region subject to foreign laws may be accessible to foreign governments or vulnerable to seizure. Distributed storage across multiple regions can complicate audit logging and control enforcement. State and international laws layer additional requirements: California’s Consumer Privacy Rights Act imposes obligations on residents’ data; Europe’s General Data Protection Regulation (GDPR) restricts cross‑border transfers; India’s data protection law may require mirroring or local retention. Effective data residency planning ensures that wherever ePHI resides, it remains protected, auditable and legally controlled.
Effective planning ensures these protections follow the data wherever it travels.
Essential concepts: residency, sovereignty, localisation and security
Understanding the difference between key concepts helps compliance leaders design architectures that meet overlapping laws:
- Data residency refers to the physical location where data is stored or processed.
- Data sovereignty deals with jurisdictional control: data is subject to the laws of the country in which it resides. Paubox notes that information stored outside the United States falls under the legal jurisdiction and data protection rules of that country.
- Data localisation is a legal requirement to keep data within certain borders. The HIPAATimes explains that some countries may require organisations to mirror or retain health data locally. HIPAA does not impose localisation, but other statutes might.
HIPAA Data Residency planning sits at the intersection of these concepts. It acknowledges that, while HIPAA allows cross‑border storage, other laws may restrict it. A good strategy also recognises that privacy is not merely about where data resides but how it is secured.
Understanding how residency, sovereignty and localisation overlap helps leaders negotiate BAAs, design cloud architectures and respond to regulators. For example, data stored in Europe is subject to the GDPR, which restricts transfers to the U.S. unless a lawful basis exists. Some jurisdictions—such as India or certain U.S. states—may impose localisation or mirroring for health data. Recognising these obligations upfront avoids costly redesigns later.
Securing health information
Protecting patient privacy requires layered technical controls. Strong encryption, access management and audit trails form the technical bedrock. Paubox notes that data sovereignty influences where encryption secrets are stored and who has access. HIPAA Data Residency planning therefore must pair location decisions with robust security measures.
Cloud governance and shared responsibility
Most healthcare providers use cloud services to scale operations. Under the shared responsibility model, the cloud provider secures the underlying infrastructure, while the customer secures configurations, identity management, encryption and monitoring. HIPAA’s risk management requirements extend into this environment: covered entities must configure services correctly, restrict regional replication and monitor for drift. Selecting vendors that offer region‑locking capabilities and strong BAA terms is crucial. Residency management is not just about contractual commitments; it is about implementing and continuously operating the controls needed to meet them.
Why a HIPAA Data Residency strategy matters
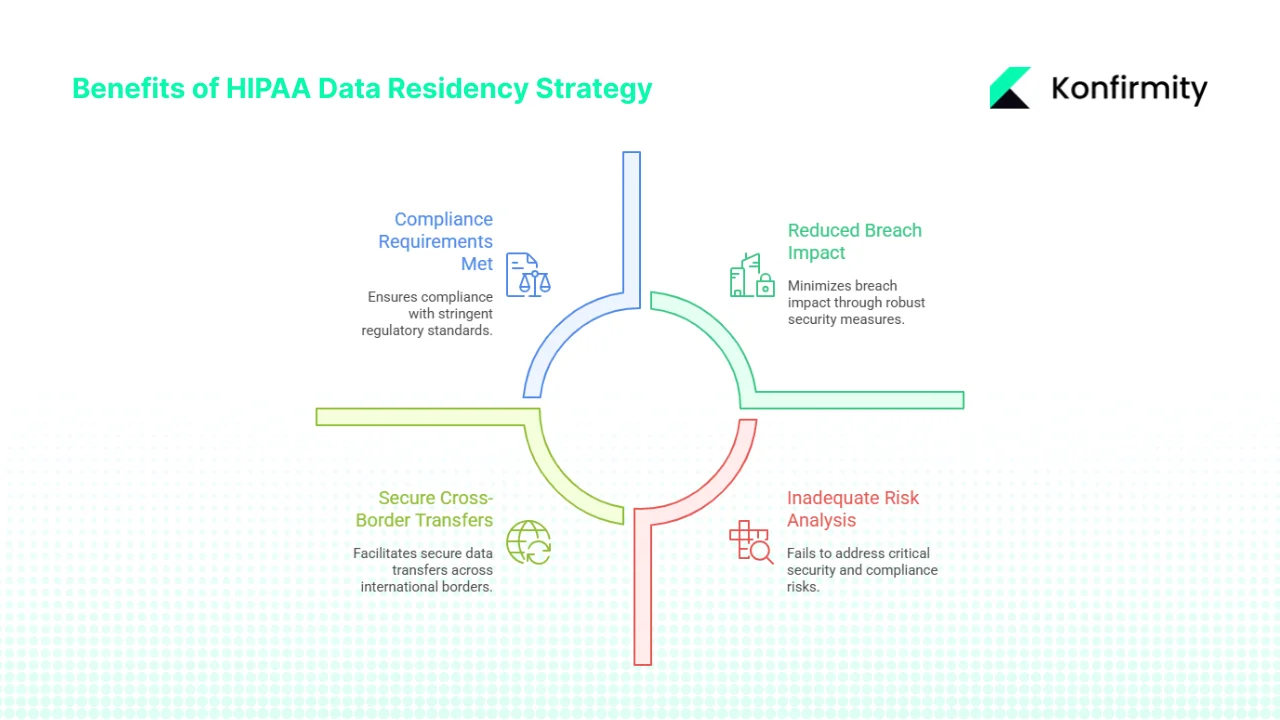
1) Protect patient privacy and reduce breach impact
Breach statistics show why residency planning is not an academic concern. Between 2009 and 2024, there were 6,759 healthcare data breaches involving at least 500 records, exposing more than 846 million individuals—a number over twice the U.S. population. IBM’s 2025 Cost of a Data Breach report found that the average cost of a U.S. data breach reached $10.22 million, a 9 % increase from the previous year. Healthcare remained the costliest industry, with breaches taking an average of 279 days to detect and contain. A well‑designed residency plan reduces the number of regions storing sensitive data, making it easier to detect and contain incidents. Restricting location, encrypting data and enforcing access controls narrows the attack surface and shortens breach lifecycles.
2) Meet compliance requirements and accelerate audits
Regulators expect documented evidence that security controls operate effectively. The Office for Civil Rights’ enforcement activities are increasing: in 2024 the agency closed 22 investigations with financial penalties. Many of those cases hinged on inadequate risk analysis and poorly documented security measures. This residency planning simplifies evidence collection because you know which regions host ePHI, what controls are applied and who is responsible. When auditors ask for proof, you can produce logs and configurations without scrambling to trace data flows. A clear residency policy also helps map HIPAA safeguards to other frameworks such as SOC 2 and ISO 27001, accelerating procurement and due diligence.
3) Manage secure cross‑border transfers
Cross‑border data transfers introduce legal and security challenges. HIPAA allows storing data outside the United States, but organisations must ensure that protections follow the data wherever it travels. Residency planning includes policies for data transit—encryption, secure protocols, and transfer minimisation—along with legal assessments to ensure that standard contractual clauses or other transfer mechanisms satisfy foreign laws. By planning this upfront, healthcare providers avoid last‑minute surprises when entering new markets or contracting with international research partners.
4) Support multi‑state and global operations
Telehealth and research organisations often operate across numerous U.S. states and multiple countries. Each jurisdiction imposes its own rules. Without a coherent residency strategy, teams risk commingling data subject to incompatible regulations. A well‑designed plan segments environments by region, ensures that local laws (e.g., state privacy statutes or GDPR) are respected and aligns with payer contract requirements. Such segmentation also improves availability and performance for patients by keeping data close to them.
Challenges and practical solutions
Despite its benefits, implementing a residency programme is not trivial. Without a structured plan, we often see access control drift, vendor sprawl, stale evidence during observation windows and weak logging. Organisations face common challenges related to technology, law and operational capacity. Based on our delivery of more than 6,000 audits and decades of experience, the following table pairs these challenges with pragmatic solutions:
Though these measures add overhead, they pay off. Human‑led managed services implement controls, monitor them and prepare evidence year‑round. Konfirmity’s “outcome as a service” model avoids compliance manufacturing and builds security that stands up during incidents and buyer due diligence.
These obstacles underline that HIPAA Data Residency should be part of a broader compliance strategy. In our experience supporting more than 6,000 audits across HIPAA, SOC 2 and ISO 27001, organisations that implement real controls see tangible benefits. Typical SOC 2 Type II readiness can shrink from nine to twelve months to four to five months, and internal effort can drop from 550–600 hours to around 75 hours per year when using a managed partner. By mapping HIPAA safeguards to other frameworks and building reusable evidence flows, teams reduce duplicate work and accelerate enterprise sales cycles.
Putting solutions into action
To bring these controls to life, follow a pragmatic roadmap:
- Map and classify data – Identify every system and region holding ePHI or related data. Tag resources to enforce region policies and support HIPAA Data Residency.
- Configure providers and agreements – Select vendors that offer region‑locking and configure storage to restrict replication. Negotiate BAAs that specify permitted regions and require notification before cross‑region transfers.
- Encrypt and control access – Apply strong encryption at rest and in transit, store cryptographic secrets securely, enforce multi‑factor authentication and use tokenisation to isolate sensitive elements.
- Monitor and audit continuously – Use cloud logs and third‑party tools to track data movement and access, set alerts for cross‑region events and automate evidence collection for HIPAA Data Residency and SOC 2 audits.
- Train and partner – Provide practical training on residency policies and engage a human‑led managed service to implement, monitor and report on controls, reducing internal effort and accelerating readiness.
With managed help, SOC 2 Type II readiness can often be achieved in four to five months versus nine to twelve months when self‑managed. The result is fewer audit findings, shorter buyer assessments and reduced breach impact.
Case examples and enabling tools
Consolidating storage into approved regions
A large hospital network migrating from on‑premises systems to the cloud initially used default multi‑region replication. A pre‑audit assessment revealed that backups were stored in Europe, subjecting the organisation to GDPR. We reconfigured storage to limit replication to U.S. regions and updated agreements to specify permitted locations. The redesign also improved backup performance and reduced storage costs. The hospital passed its HIPAA risk analysis review and secured an enterprise contract that required proof of compliant data residency.
Segmenting data across borders
A telehealth provider serving patients across the U.S. and Canada replicated recordings to Asia for analytics, violating provincial restrictions. They corrected this by keeping U.S. data in U.S. regions, processing Canadian data in Canada with separate access controls, and using de‑identified data for analytics. Updated BAAs and transfer logs satisfied auditors.
Tools to simplify management
Several categories of tools make data residency easier to manage:
- Data governance platforms map data flows and enforce location policies across clouds.
- Monitoring tools track resource configurations and alert when data moves outside approved regions.
- Compliance dashboards collect evidence and generate auditor‑ready reports; managed services provide “outcome as a service” aligning HIPAA, SOC 2 and ISO 27001.
Conclusion
HIPAA does not dictate a storage country; it requires protecting ePHI wherever it resides through risk analysis, access control, encryption and legal agreements. With enforcement rising and breach costs climbing, HIPAA Data Residency has become a strategic security issue. A durable plan—mapping data flows, enforcing regional controls, negotiating clear BAAs, encrypting, monitoring and training—helps organisations meet HIPAA, SOC 2 and ISO 27001 requirements and reduces breach impact. Security that works in practice matters more than paperwork. Start with security, operate it daily, and compliance follows. Managed, human‑led services ensure controls remain effective and current.
Frequently asked questions
1. Does HIPAA mandate where data must be stored?
No. HIPAA focuses on security and privacy safeguards; location choices are governed by other laws and risk considerations.
2. Is cloud storage allowed for ePHI?
Yes, provided encryption, access controls and a business associate agreement are in place.
3. What’s the difference between data residency and data localisation?
Data residency concerns where data lives; data localisation is a legal requirement to keep data within certain borders. HIPAA does not impose localisation, but other laws such as GDPR may.
4. Can ePHI be stored outside the United States?
Yes, but appropriate safeguards must be in place and the organisation must follow applicable laws.
5. What should be included in a business associate agreement? \
Specify permitted regions, require encryption and access controls and define incident reporting.




.svg)





.svg)
.svg)