Most enterprise buyers now ask for security assurance artifacts before finalising contracts. In health‑care, the stakes are even higher because systems store electronic protected health information (ePHI) and must satisfy the U.S. Health Insurance Portability and Accountability Act (HIPAA). Robust HIPAA Vulnerability Management is no longer optional – it is essential for protecting patient data, maintaining business operations, and keeping deals on track. The HIPAA Security Rule requires covered entities and their business associates to assess risks, implement safeguards and demonstrate due diligence. Recent regulatory proposals go further, calling for regular vulnerability scanning, penetration testing and technology asset inventories. This article explains what that means in practice, how Konfirmity implements it, and why health‑care leaders should start with security and arrive at compliance.
Why Vulnerability Management Matters in Health‑Care
Health‑care providers have been the most expensive industry to breach for 14 consecutive years. IBM’s 2025 Cost of a Data Breach report shows that U.S. data breaches cost an average of $10.22 million, up 9.2 % from 2024. The average cost of a health‑care breach fell to $7.42 million, but it remains the costliest of all industries. Attacks now cripple hospital operations through ransomware, supply‑chain exploits and third‑party compromises. The time to identify and contain a health‑care breach averages 279 days—five weeks longer than the global average. OCR enforcement actions highlight the risks: in 2025 the Office for Civil Rights (OCR) imposed a $1.5 million civil monetary penalty on Warby Parker for failing to conduct a risk analysis and manage vulnerabilities. Eight enforcement actions under the OCR’s Risk Analysis Initiative have already collected nearly $900 000 in settlements. Managing vulnerabilities proactively is therefore not just a best practice—it’s a regulatory mandate and a business imperative.
What Is HIPAA Vulnerability Management?
HIPAA Vulnerability Management refers to a structured process for identifying, prioritising, mitigating and monitoring security weaknesses in systems that create, receive or transmit ePHI. While general cybersecurity programs use vulnerability scanning and patch management, HIPAA ties those activities to specific obligations under the Security Rule. Covered entities must conduct an accurate and thorough risk analysis of potential threats and vulnerabilities to the confidentiality, integrity and availability of all ePHI, implement security updates, and correct identified deficiencies. This duty covers all forms of electronic media—hard drives, portable devices, transmission media and cloud environments. The HIPAA Security Rule currently distinguishes between “required” and “addressable” implementation specifications, but a 2024–25 Notice of Proposed Rulemaking (NPRM) would make all specifications mandatory and require detailed documentation, asset inventories, vulnerability scans every six months and annual penetration testing.
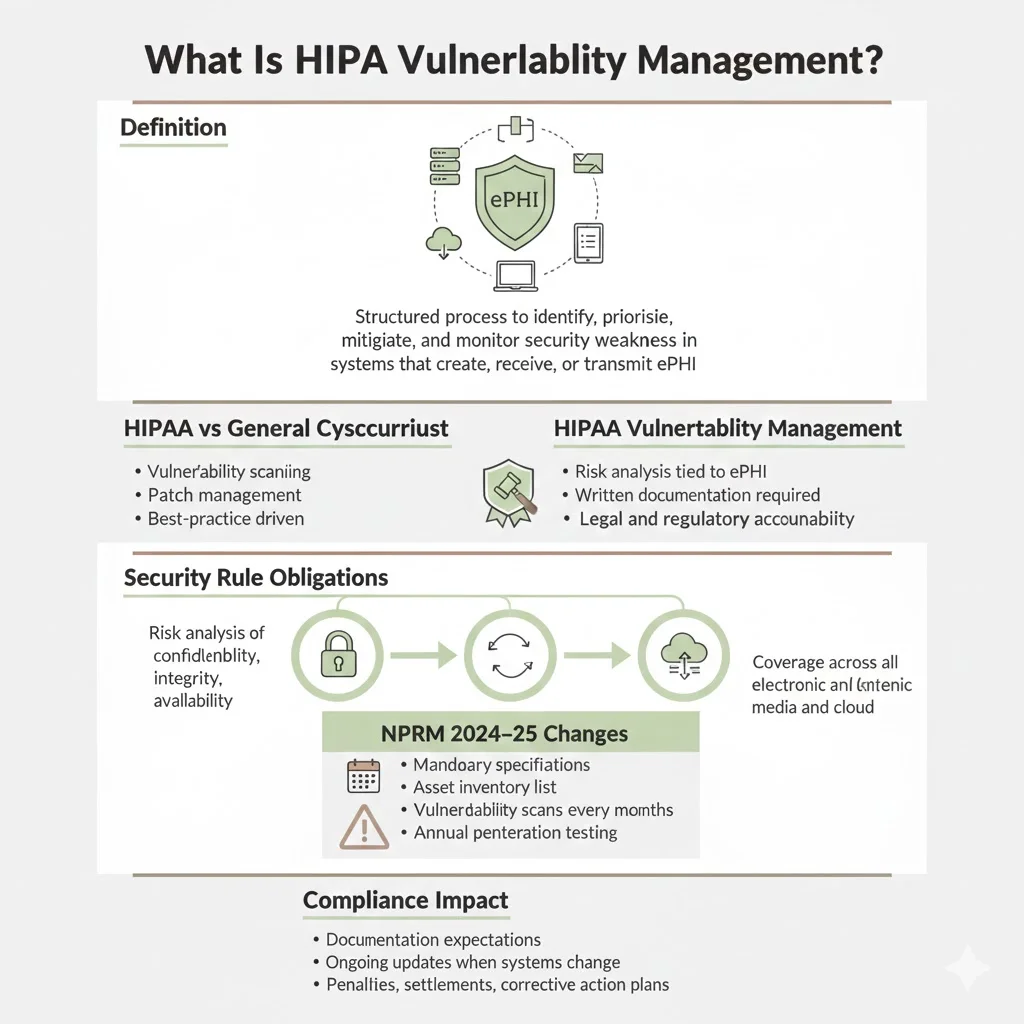
HIPAA vulnerability management differs from general cybersecurity by emphasizing ePHI and legal accountability. The risk analysis must be documented and updated whenever systems change, and covered entities must document policies, procedures and analyses. Failure to comply can lead to civil monetary penalties, settlements and corrective action plans.
Core Regulatory and Compliance Foundations
A. HIPAA Security Rule Basics
The Security Rule is organized into three categories of safeguards:
- Administrative safeguards: risk analysis, risk management, sanction policies and workforce training. These measures require identifying and evaluating risks to ePHI and implementing policies to reduce them.
- Physical safeguards: facility access controls, workstation use policies and device/media controls. Physical protections prevent unauthorized access to systems and media containing ePHI.
- Technical safeguards: access controls, audit controls, integrity controls and transmission security. These include encryption of ePHI in transit and at rest, unique user identifiers, automatic logoff and audit logging.
The NPRM proposes to remove the “addressable” category and make all implementation specifications mandatory. It also requires multi‑factor authentication, network segmentation, anti‑malware, vulnerability scanning every six months and annual penetration testing. Encryption of ePHI at rest and in transit would become explicitly required.
B. Risk Assessment and Risk Management
The HIPAA Security Rule requires covered entities to perform a risk analysis and implement a risk management program. Key steps include:
- Collection of relevant data: inventory of information assets, data flows and system interfaces. NIST SP 800‑30 describes preparing for a risk assessment by establishing context, scope, assumptions, information sources and analytic approaches.
- Identification of threats and vulnerabilities: identify reasonably anticipated threats, vulnerabilities and predisposing conditions to systems handling ePHI. NIST’s risk assessment process emphasises identifying threat sources and events, vulnerabilities, likelihood, and potential impact.
- Assessment of security measures: determine existing controls, identify gaps and evaluate their effectiveness. Determine the likelihood of exploitation and the magnitude of impact.
- Threat likelihood & impact analysis: assign risk levels based on likelihood and impact to prioritise remediation. NIST SP 800‑30 provides detailed guidance on calculating risk.
- Documentation and ongoing review: document the risk assessment findings, communicate them to decision makers and maintain them over time. HIPAA requires updates whenever systems change or new vulnerabilities emerge.
C. Compliance Auditing
Periodic auditing is essential to demonstrate compliance. The NPRM would require regulated entities to conduct a compliance audit at least once every 12 months. Auditors examine whether the entity has performed and documented risk analyses, vulnerability scans, penetration tests and corrective actions. In the SOC 2 context, Trust Services Criterion CC7.1 requires vulnerability scanning after significant changes and on a periodic basis. Modern auditors expect evidence of both vulnerability scanning and penetration testing; a 2024 survey found 67 % of organisations without regular scanning received management letter comments.
Step‑by‑Step HIPAA Vulnerability Management Process
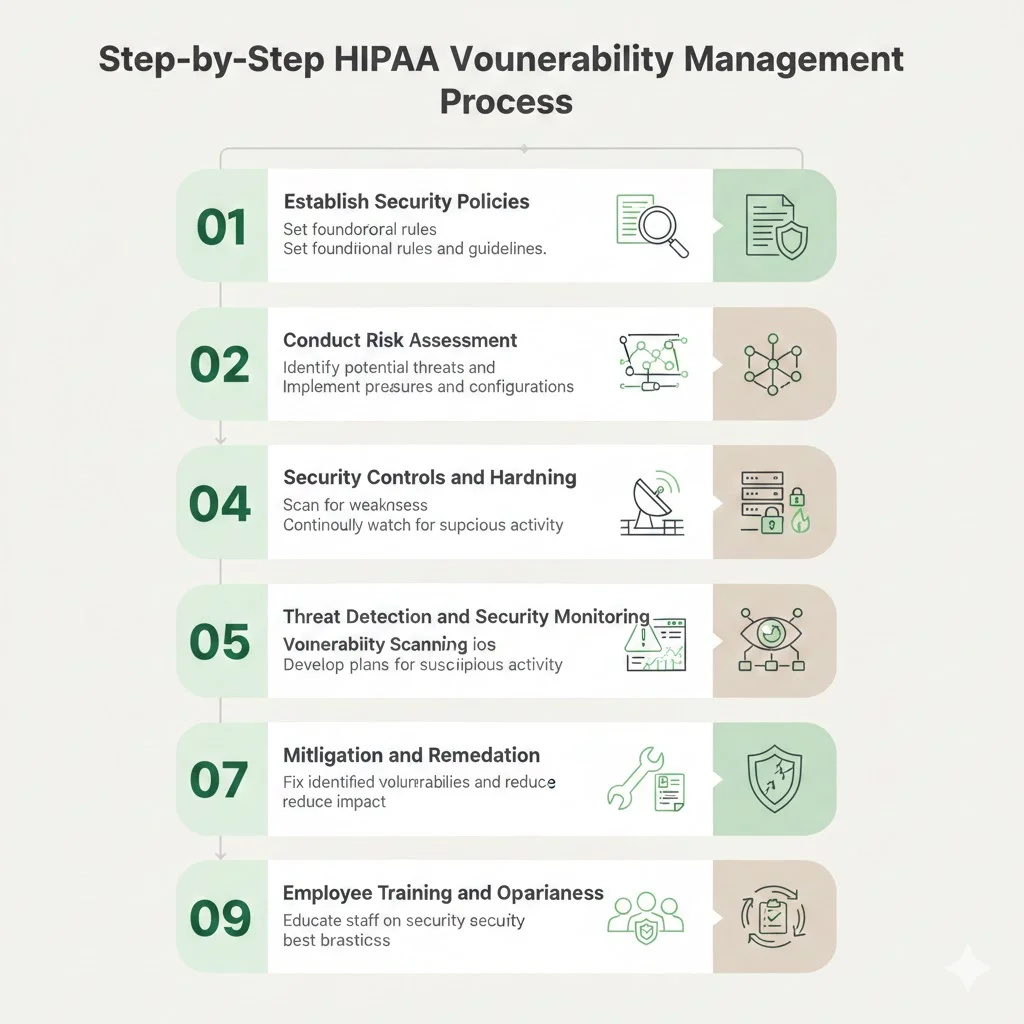
Step 1: Establish Security Policies
Define policies governing vulnerability scanning, patching, access control and monitoring. Document roles, responsibilities and escalation paths. HIPAA requires written documentation of all Security Rule policies, procedures and analyses. Policies should reference other frameworks when appropriate—ISO 27001 Clause 12.6.1 requires obtaining information on technical vulnerabilities in a timely fashion, evaluating exposure and taking appropriate measures. In practice, Konfirmity’s team drafts policies aligned with the organization’s technology stack, regulatory obligations and business objectives. We emphasise continuous improvement: policies are reviewed quarterly to incorporate new threat intelligence and lessons from audits.
Step 2: Conduct Risk Assessment
Identify ePHI assets and entry points. Document data flows, system interfaces, third‑party integrations and storage locations. Catalog known and potential vulnerabilities using vendor advisories, CVE feeds and threat intelligence. Prioritise based on risk level—consider exposure, asset importance, potential impact, severity scores (CVSS) and likelihood. NIST’s risk assessment process includes preparing for the assessment, conducting it, communicating results and maintaining it. The NPRM would require reviewing the technology asset inventory and network map and identifying anticipated threats and vulnerabilities. Our experience shows that high‑impact vulnerabilities are often found in overlooked systems—legacy MRI scanners, network‑attached storage or vendor‑managed EHR modules. Konfirmity’s risk assessments typically take 2–3 weeks and feed directly into remediation plans.
Step 3: Security Controls and System Hardening
Apply technical controls to reduce risk. Use firewalls and virtual private networks to isolate clinical networks. Encrypt ePHI at rest and in transit; the NPRM would make encryption mandatory. Implement multi‑factor authentication across all systems containing ePHI. Restrict access using least‑privilege principles and review permissions quarterly. Apply role‑based access control and log administrative actions. Harden endpoints by removing unnecessary software and disabling unused ports. Patch operating systems, firmware and applications promptly; ISO 27001 Clause 12.6.1 requires timely remediation of technical vulnerabilities. Our audits often reveal patch management pitfalls: teams may rely on manual processes, leaving unpatched devices for months. Automation and SLA tracking reduce the median time to patch (MTTP) from 30 days to under two weeks.
Step 4: Vulnerability Scanning
Vulnerability scanning uses tools to detect known weaknesses in systems and software. SOC 2 auditors interpret Criterion CC7.1 to require vulnerability scans on a periodic basis and after significant changes. The HIPAA NPRM would require vulnerability scanning at least every six months. For high‑risk environments, Konfirmity schedules monthly internal scans and quarterly external scans. Tools like Nessus, Rapid7 InsightVM and Qualys quickly identify missing patches, misconfigurations and outdated encryption protocols. Scans should cover workstations, servers, network devices, cloud environments and medical devices. Align scanning frequency with change management; weekly scans for dynamic systems and after major deployments. Document findings and feed them into the remediation pipeline.
Step 5: Threat Detection and Security Monitoring
Continuous monitoring is critical for catching emerging threats. Use security information and event management (SIEM) platforms to aggregate logs from endpoints, servers, firewalls and EHR applications. Network monitoring tools detect anomalous traffic patterns, lateral movement and exfiltration attempts. Integration with vulnerability scanning provides a holistic view: events can be correlated with known weaknesses to prioritise responses. NIST’s vulnerability management framework emphasises continuous monitoring and incident alerts. Konfirmity uses managed detection and response (MDR) services to provide 24/7 coverage; we deliver threat intelligence and alert triage to security teams.
Step 6: Incident Response Preparedness
Vulnerabilities often surface during incidents. Incorporate vulnerability findings into incident response playbooks. Define thresholds for escalation (e.g., high‑severity vulnerabilities exploited in the wild). Create step‑by‑step procedures for containing an exploit, preserving forensic evidence and notifying stakeholders. The HIPAA NPRM proposes requiring written security incident response plans and procedures. Regular tabletop exercises and red‑team simulations build muscle memory. Konfirmity’s clients run quarterly drills that integrate vulnerability data, ensuring teams can respond swiftly when an exploit emerges.
Step 7: Mitigation and Remediation
Prioritise and remediate vulnerabilities based on risk. The NIST process involves identification, assessment, mitigation, remediation, verification and continuous monitoring. Address critical vulnerabilities affecting Internet‑exposed assets immediately. Apply security patches, configuration changes or compensating controls. For vulnerabilities that cannot be patched quickly, isolate affected systems, restrict network access or monitor intensively. Document actions, track status and verify that fixes were effective. Use risk‑based SLAs—high‑severity issues resolved within seven days, medium severity within 30 days, and low severity within 90 days. Automation can accelerate deployment and reduce human error.
Step 8: Employee Training and Awareness
People remain a critical factor in vulnerability management. Phishing, social engineering and misuse of credentials are common attack vectors. Train employees on recognising phishing attempts, handling ePHI securely, reporting anomalies and following access control policies. The HIPAA Security Rule requires workforce security awareness and training; ISO 27001 Clause 7.3 emphasises competence. Regular training reduces the likelihood of credential theft and shortens breach detection time. Encourage a culture of security by recognising employees who report potential issues.
Step 9: Ongoing Review and Optimization
Vulnerability management is a continuous cycle. Reassess the environment after remediation and verify that vulnerabilities are closed. Update risk analyses when new systems are deployed, when vulnerabilities are discovered or when threat actors change tactics. Document improvements and lessons learned. Conduct periodic internal audits and annual external audits to ensure controls remain effective. Continuous improvement ties directly to compliance and breach prevention; it demonstrates due diligence to auditors, regulators and business partners.
Measuring Success: Metrics & Reporting
Robust metrics help organisations track progress and demonstrate compliance. Important key performance indicators (KPIs) include:
Reporting structures should align with executive and audit requirements. Provide dashboards to CISOs, CIOs and compliance officers, with roll‑up summaries for boards. Use risk scoring and trend analysis to prioritise investment. Include metrics in quarterly business reviews and procurement questionnaires to accelerate buyer due diligence.
Tools and Technologies to Support HIPAA Vulnerability Management
Selecting the right tools can streamline vulnerability management. Key categories include:
- Vulnerability scanners (e.g., Nessus, Qualys, Rapid7 InsightVM): automate discovery of missing patches, misconfigurations and outdated software. Provide CVSS scoring and integration with ticketing systems.
- Penetration testing platforms: simulate attacks to validate controls under adversarial conditions. SOC 2 auditors expect penetration testing evidence to demonstrate control effectiveness. Konfirmity uses human‑led testing complemented by automated tools to uncover deeper issues.
- Security information and event management (SIEM) tools: aggregate logs, correlate events and generate alerts. Integrate with vulnerability scanning to connect exploits with known weaknesses.
- Asset inventory and network mapping: maintain real‑time inventories and network maps to support risk assessment and NPRM requirements.
- Configuration management and patching platforms: deploy updates across diverse environments; enforce baselines and track compliance.
- GRC and risk dashboards: centralise evidence, track controls and provide auditor‑ready documentation. Konfirmity’s platform delivers dashboards that show control status, open vulnerabilities, SLA metrics and audit readiness.
Automation and integration are critical. Tools should integrate with CI/CD pipelines to catch vulnerabilities before production, support API access for custom workflows, and generate reports aligned with HIPAA, SOC 2 and ISO 27001 requirements.
Common Challenges and How Healthcare Teams Overcome Them
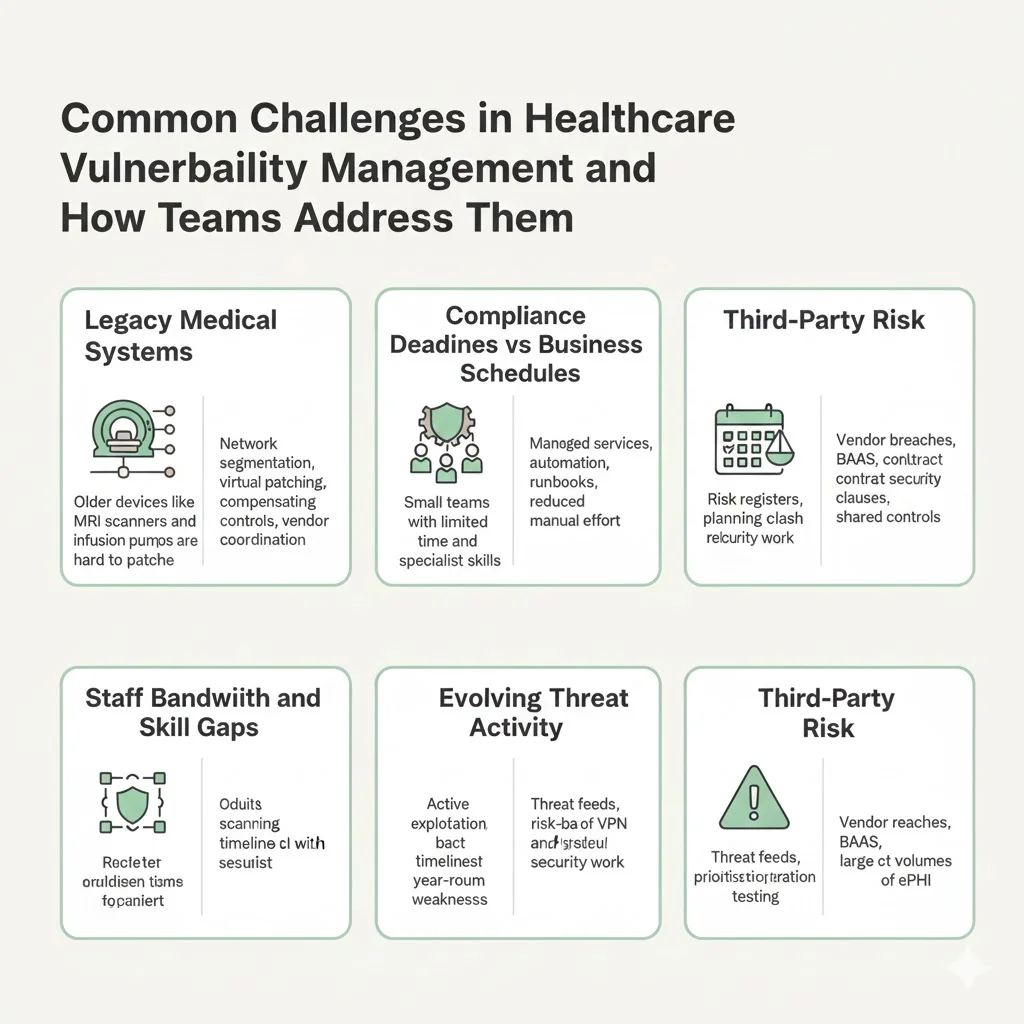
- Legacy medical systems: Many health‑care organisations rely on legacy devices such as MRI scanners and infusion pumps that are difficult to patch. Mitigations include network segmentation, virtual patching, compensating controls and vendor coordination. The NPRM proposes requiring network segmentation and backup controls.
- Staff bandwidth and skill gaps: Security teams are often understaffed. Managed services like Konfirmity provide dedicated experts to execute vulnerability management, reducing internal effort from hundreds of hours to ~75 hours per year. Automation and runbooks shorten remediation cycles.
- Alignment with compliance deadlines: Regulatory timelines (e.g., annual audits, six‑month scanning requirements) can collide with product release schedules. Use project management and risk registers to align security work with business cycles. Konfirmity emphasises year‑round operations instead of one‑off projects.
- Evolving threat landscape: Attackers exploit unpatched vulnerabilities in VPNs and firewalls; Verizon’s 2025 DBIR found vulnerability exploitation accounted for 20 % of breaches and that only 54 % of critical vulnerabilities were fully patched, with a median fix time of 32 days. Stay ahead by subscribing to threat intelligence feeds, prioritising high‑risk vulnerabilities and testing defences through penetration testing.
- Third‑party risk: Mega breaches often originate from third‑party vendors; the Change Healthcare incident exposed 190 million records. Perform vendor risk assessments, require business associate agreements (BAAs) and include vulnerability management clauses in contracts. SOC 2 and ISO 27001 frameworks support re‑using controls across vendor assessments.
Conclusion
HIPAA Vulnerability Management is the linchpin of secure, compliant health‑care operations. The cost of a data breach remains astronomical, and regulators are tightening requirements. The NPRM proposes mandatory vulnerability scans, penetration tests, technology asset inventories and written documentation. OCR’s Risk Analysis Initiative has already produced settlements nearing $900 000, and fines can reach $71 162 per violation. Proactive vulnerability management—grounded in risk assessments, continuous scanning, rapid remediation, rigorous documentation and regular audits—reduces the likelihood of breaches, accelerates sales cycles and satisfies regulators. At Konfirmity, we start with security and arrive at compliance. Our human‑led, managed security and compliance service implements controls inside your stack, monitors them year‑round and keeps you audit‑ready so you can focus on delivering care.
Frequently Asked Questions
1. What does HIPAA Vulnerability Management mean?
HIPAA vulnerability management is a structured process for identifying, assessing, prioritising and mitigating security weaknesses in systems that handle electronic protected health information. It ties general vulnerability management practices to the HIPAA Security Rule, requiring documented risk analyses, timely remediation and continuous monitoring.
2. Do you have to do vulnerability scans for HIPAA?
The current Security Rule does not explicitly state a scanning interval, but covered entities must assess potential risks and vulnerabilities to ePHI and implement safeguards. The 2024–25 NPRM would mandate vulnerability scanning at least every six months and penetration testing annually. SOC 2 auditors already expect periodic scans and evidence of remediation.
3. How often should risk assessments be performed?
HIPAA requires risk assessments to be conducted when systems change and periodically thereafter. NIST recommends a four‑step process—prepare, conduct, communicate and maintain—and emphasises ongoing updates. Many organisations perform a comprehensive assessment annually with interim updates when material changes occur. The NPRM proposes requiring an annual compliance audit.
4. What’s the difference between vulnerability scanning and penetration testing?
Vulnerability scanning uses automated tools to detect known weaknesses; penetration testing simulates real‑world attacks to validate whether controls can withstand exploitation. SOC 2 Criterion CC7.1 requires vulnerability scans on a periodic basis, while auditors increasingly expect penetration testing evidence to prove control effectiveness. The HIPAA NPRM also proposes penetration tests at least once every 12 months.
5. How does vulnerability management tie to incident response?
Vulnerability findings feed directly into incident response planning. High‑severity vulnerabilities become triggers for escalation, containment and notification. The NPRM proposes requiring written incident response plans and restoration procedures. Ongoing vulnerability management ensures incident response teams are aware of current risks and can quickly address exploited weaknesses.
6. What happens if a health‑care company fails to manage vulnerabilities?
Failure to conduct a risk analysis and manage vulnerabilities can lead to significant penalties. OCR has imposed settlements and civil monetary penalties ranging from $5 000 to $3 million for risk analysis failures. Warby Parker received a $1.5 million penalty in 2025 for risk analysis and risk management violations. Beyond fines, unaddressed vulnerabilities expose organisations to costly breaches averaging $7.42 million and can disrupt patient care.
7. Are there automated tools that help with HIPAA Vulnerability Management?
Yes. Vulnerability scanners, SIEMs, patch management platforms and GRC dashboards automate discovery, prioritisation and reporting. SOC 2 auditors expect evidence generated by automated scanning and penetration testing tools. Konfirmity leverages integrated toolchains to provide real‑time visibility, automate remediation workflows and maintain audit‑ready evidence.





.svg)




.svg)
.svg)