Most enterprise buyers now request proof of security before signing contracts. Healthcare partners will not move forward until a provider can show that protected health information (PHI) is safe and that privacy controls are in place. Being ready for an audit goes far past filling out a checklist. It means running security controls day‑to‑day and collecting evidence continuously. In this article I’ll unpack what a HIPAA audit is, why budgeting matters, and how different cost components add up. The discussion is grounded in data from recent guidance and reflects practical lessons from running more than 6,000 audits over 25 years. The phrase HIPAA Audit Cost appears several times because that is what you are probably searching for. Understanding your HIPAA Audit Cost early helps you allocate budget effectively. Your first takeaway: an audit is not a trivial expense, but proactive budgeting is still less costly than remediation and fines.
What is a HIPAA audit?
Under the Health Insurance Portability and Accountability Act, the Office for Civil Rights (OCR) has authority to investigate how covered entities and business associates handle PHI. A HIPAA audit is a structured assessment of your security, administrative and physical safeguards. Auditors review risk management practices, verify that you follow the Privacy and Security Rules, and ensure that breaches and requests for records are handled correctly. There is no formal certification program baked into HIPAA; instead, OCR uses audits and investigations to enforce compliance. Audits happen for several reasons: some are part of the random audit cycle launched by OCR, others follow a complaint or a breach report. The intensity can vary. A desk audit is a remote document review that focuses on specific controls and may require only limited evidence. An onsite audit is much deeper. It involves in‑person interviews, walk‑throughs of facilities and system reviews, and can span several days.
As a practitioner, I see many organizations view audits as optional. They are not. Although the law does not require certification, OCR expects organizations to conduct periodic risk assessments and implement appropriate safeguards. In practice, many healthcare providers hire third‑party auditors to perform a readiness assessment or a full compliance audit so they can identify gaps before OCR calls. Understanding the cost of these activities helps leaders allocate resources appropriately.
Why understanding HIPAA audit cost matters
Compliance is not a single project. It is an ongoing security program that intersects with patient care, procurement, and business growth. Audit costs are one piece of this program. Direct costs include auditor fees, risk assessments and consultant charges. Indirect costs include the hours your team spends gathering documentation, training staff, and updating policies. Overlooking these expenses or viewing them as secondary can lead to underinvestment in safeguards. A mid‑range estimate for achieving HIPAA compliance in 2024 was between $80,000 and $120,000, and the range depends heavily on whether most of the work is done in‑house or outsourced. Those figures cover more than just an audit; they include ongoing risk management, monitoring, and training. By contrast, the fines for non‑compliance can easily exceed what you would spend on preparedness. OCR uses a tiered penalty structure where fines start at $141 per violation and climb to more than $71,000 per violation depending on negligence. Criminal cases involve fines up to $250,000 plus possible prison time. Those fines are assessed per violation, and annual caps can exceed $2 million.
Apart from monetary penalties, a breach can disrupt operations and damage trust. IBM’s 2025 Cost of a Data Breach Report, summarized by the HIPAA Journal, reported that the average healthcare breach in the United States cost $7.42 million, with U.S. data breach costs reaching a record $10.22 million. Longer investigation and remediation periods also take staff away from patient care. When you budget for audits up front, you reduce the risk of these downstream costs.
Typical range of costs
The phrase HIPAA Audit Cost encompasses various line items, not a single fee. Below I break down common components using published ranges and our own observations. Keep in mind that numbers vary based on organization size, complexity and existing security maturity. A small telehealth startup may spend between $25,000 and $70,000 on its initial program, while an enterprise health system can easily allocate hundreds of thousands of dollars.
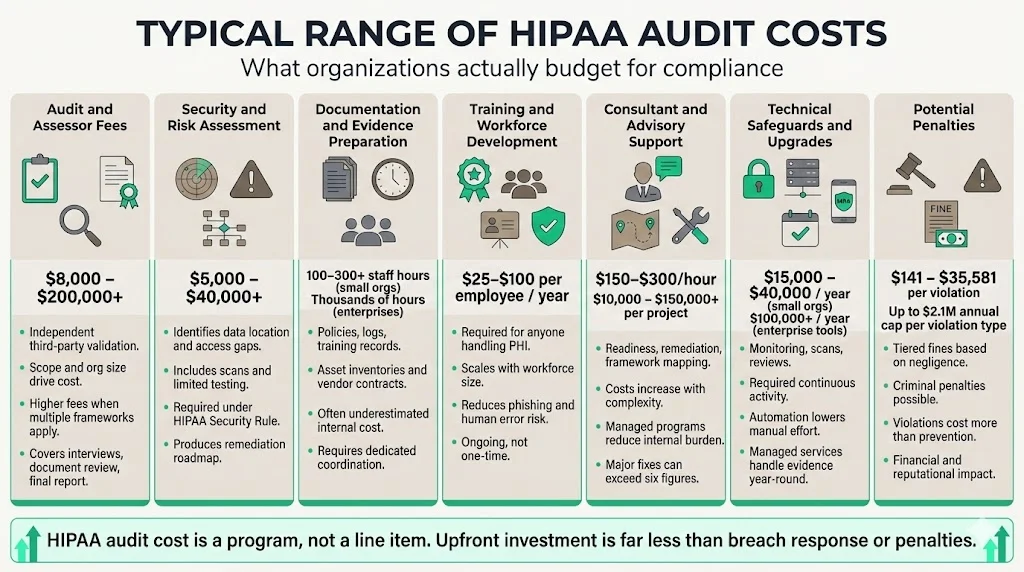
1. Audit and assessor fees
Third‑party auditors provide an independent validation of your compliance. They review documentation, interview staff and produce a report. Fees are typically tied to the size and scope of your organization. Thoropass’ HIPAA cost guide states that auditor fees range from $15,000 to $200,000+ depending on complexity. A small clinic may engage a part‑time consultant for a focused assessment costing around $8,000–$25,000, while a multi‑site healthcare system may pay six figures for a full onsite audit. These fees cover assessor time, document review, and final reporting. Assessors may also charge more when multiple frameworks (HIPAA plus HITRUST or SOC 2) are in scope, because coordination and evidence mapping increase effort.
2. Security and risk assessment
A risk analysis identifies where sensitive data resides, who can access it, and which controls are missing. External risk assessments generally range from $5,000 to $20,000 according to DSALTA’s 2025 cost guide. Thoropass provides a similar range, stating that readiness assessments start at $5,000 for small organizations and can exceed $40,000 for larger ones. For startups, the cost includes vulnerability scanning and some penetration testing; for hospitals it often involves technical architecture reviews, interviews with clinicians and system administrators, and sampling of devices and medical applications. The deliverable is a report listing gaps and proposed remediations. These assessments are not optional. OCR expects covered entities and business associates to perform regular risk analyses under the Security Rule.
3. Documentation review and evidence preparation
HIPAA compliance requires policies for privacy, security, breach notification, contingency plans, device management, and business associate agreements. Gathering and reviewing these documents consumes staff time. Many providers underestimate this effort. The bigger the organization, the more complex the documentation. You will need to collect access logs, training records, incident response plans, asset inventories, encryption proof, and vendor contracts. Although there is no direct line item like a consultant fee, the labor cost is real. In our experience supporting 6,000+ audits, small organizations spend 100–300 person‑hours preparing evidence. Larger systems may spend thousands of hours across multiple departments. Budget for this by assigning dedicated compliance coordinators or using managed services that handle evidence collection throughout the year.
4. Training and workforce development
Every person who touches PHI needs to understand privacy and security obligations. The cost of training depends on workforce size and delivery method. Virtual Sprout’s 2025 guide reports that annual HIPAA risk assessments typically cost $3,000–$10,000 and that organizations spend $25–$100 per employee on security training. For a 30‑clinician mental health practice, total training costs might run $2,000–$5,000, while a health system with thousands of staff may invest tens of thousands per year. Regular training reduces the likelihood of phishing and social engineering incidents, which remain common triggers for breaches.
5. Consultant assistance
Many healthcare providers hire compliance consultants to design controls, map requirements across frameworks (HIPAA, SOC 2, ISO 27001, GDPR), and guide remediation. Consultant rates vary widely—hourly rates range from $150 to $300, and project‑based engagements can cost $10,000 to $150,000 depending on scope. Thoropass states that remediation work can range from minor fixes costing $1,000 to major architectural changes exceeding $200,000. Consultants often provide a readiness assessment followed by remediation oversight. At Konfirmity, we distinguish ourselves by embedding a dedicated CISO and compliance team to run the program year‑round rather than handing over a report and walking away. This managed service approach reduces internal effort by 75% compared with self‑managed programs and ensures that controls are continuously operated.
6. Technical safeguards and upgrades
Technical measures are the backbone of HIPAA compliance: encryption at rest and in transit, multi‑factor authentication (MFA), secure backups, log management, and network segmentation. Virtual Sprout estimates that rolling out MFA, secure email and access management costs $2,000–$10,000+. Thoropass states that technical remediation can run $20,000–$150,000 for mid‑sized practices. For an enterprise pursuing HITRUST certification, security infrastructure investments such as SIEM systems, identity controls and segmentation can push the budget into the $250,000–$5,000,000+ range. These investments not only satisfy HIPAA but also support other frameworks and reduce the risk of breaches.
7. Ongoing risk management and monitoring
Risk management is not a single event. The Security Rule requires covered entities to implement a process to regularly review records of information system activity, such as audit logs, access reports and security incident tracking. Costs include periodic vulnerability scanning, penetration tests, and risk analysis updates. For a mental health provider, annual maintenance—including monitoring, training and documentation updates—runs $15,000–$40,000. Automation tools range from $99 per month for small organizations to more than $100,000 per year for enterprise deployments. Managed services like ours handle continuous monitoring, vendor risk assessments, and evidence collection, freeing your team to focus on patient care.
8. Potential penalties
Budgeting should also account for the risk of penalties. OCR uses a four‑tier structure where fines depend on the degree of negligence. In 2025, per‑violation fines ranged from $141 to $35,581 when the organization was unaware of the violation, up to a minimum of $71,162 per violation when willful neglect was not corrected. Annual caps per violation type sit at $2,134,831. Criminal penalties, though less common, include fines up to $50,000 and prison time for knowingly obtaining or disclosing PHI, with higher penalties for offenses involving false pretenses or personal gain. These numbers illustrate why proactive investment in security is less costly than responding to a violation.
Step‑by‑step guide to estimating your costs
If you need a practical approach to plan your HIPAA Audit Cost, use the following steps. They are distilled from our work with hundreds of healthcare clients.
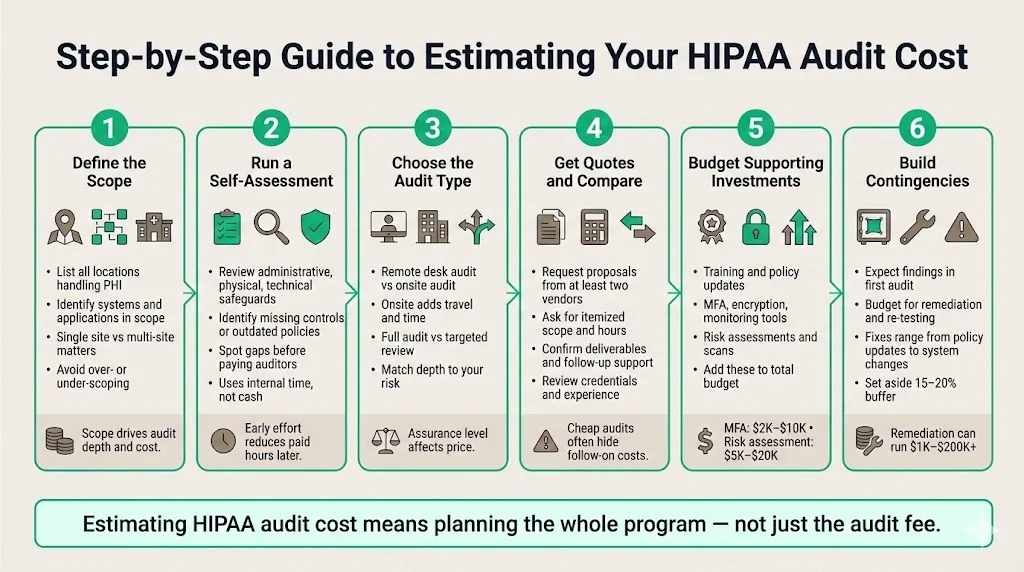
Step 1: Define the scope. List all locations, systems and applications that handle PHI. Determine whether you only need to cover a single clinic or multiple sites with varied services. Scope influences the number of controls and the depth of the audit. Overscoping inflates cost; underscoping increases risk.
Step 2: Conduct a preliminary self‑assessment. Before engaging an auditor, perform an internal review. Use the Security Rule’s administrative, physical and technical safeguard categories as your checklist. Identify obvious gaps like missing encryption, outdated policies, or lack of workforce training. This internal activity may cost nothing but your team’s time and will reduce consultant hours later.
Step 3: Choose the audit type. Decide whether you need a remote desk audit, an onsite audit, or a thorough readiness assessment. Remote audits involve document reviews and interviews via video call and are less expensive. Onsite audits provide stronger assurance but include travel and accommodation expenses for the auditor. Also decide whether you are pursuing a full compliance audit or a targeted review (for example, focusing on the Right of Access rules).
Step 4: Solicit quotes from auditors and consultants. Request detailed proposals from at least two vendors. Ask for an itemized list of scope, number of hours, deliverables, and any follow‑up support. Reputable firms should disclose whether their fees include remediation guidance or just the assessment. When comparing quotes, factor in the vendor’s experience, accreditation (e.g., HITRUST assessor, AICPA peer review) and track record.
Step 5: Plan supporting investments. In addition to auditor fees, budget for training, policy development, technical upgrades and continuous monitoring. Use the cost ranges above as a baseline. For instance, if you plan to adopt MFA, allocate $2,000–$10,000; if you need a risk assessment, reserve $5,000–$20,000. When estimating your HIPAA Audit Cost, include these supporting costs in your total. Being realistic about these supporting costs avoids unpleasant surprises.
Step 6: Build contingencies. No organization passes a first audit without findings. Include funds for remediation and re‑testing. Remediation might be as simple as revising an access control policy or as complex as implementing encryption across a legacy system. Thoropass’ guide shows remediation work ranging from $1,000 to over $200,000. Setting aside 15–20% of your estimated budget for contingencies is prudent.
Cost scenarios
To illustrate how HIPAA Audit Cost varies, here are three examples based on real engagements. All names and identifying details have been anonymized.
Example A: Small clinic. A single‑site family practice with eight employees processes appointment scheduling, basic billing and limited electronic health records. They hire a consultant for a readiness assessment costing $10,000. Their risk assessment reveals outdated anti‑virus software and missing encryption. Remediation includes purchasing a HIPAA‑compliant email service and implementing MFA ($3,000). Staff complete a web‑based training module at $50 per person. Documentation preparation and policy drafting consume 80 staff hours. The total initial budget is around $15,000, plus $3,000 annually for monitoring and training.
Example B: Mid‑sized healthcare provider. A three‑location practice with 150 employees handles a range of services including radiology, lab work and telemedicine. They commission an onsite compliance audit costing $30,000. An in‑depth risk analysis ($20,000) identifies the need for network segmentation, encryption of portable devices, and new access review processes. They invest $50,000 in technical upgrades and $7,500 in staff training. Consultant support for remediation and control design adds $25,000. The initial program costs approximately $132,500, and they budget $40,000 annually for continuous monitoring, vendor risk management and recurrent training.
Example C: Large hospital system. A regional health system with multiple hospitals, clinics and a research unit pursues HITRUST certification to satisfy payer and partner requirements. They undergo multiple audits, including HIPAA, SOC 2 and HITRUST. Assessment fees total $150,000. Risk assessments and penetration tests across hundreds of systems cost $70,000. Technical remediation (implementing SIEM, identity management and encryption at scale) reaches $1,000,000. Staff training programs for thousands of employees cost $75,000. Ongoing operations—continuous monitoring, vendor risk assessments, change management reviews, and documentation updates—require a dedicated security and compliance team. Total initial investment surpasses $1.3 million, and annual maintenance is in the mid‑six figures.
Controlling and optimizing costs
There are several practical ways to keep your HIPAA Audit Cost under control without compromising security:
- Use internal capabilities where appropriate. If you have competent IT and compliance staff, use them for evidence collection, policy drafting and initial gap analysis. This reduces consultant hours. However, avoid the false economy of assigning compliance tasks to people who lack expertise; errors during documentation can cost more later.
- Use automation tools judiciously. Modern compliance platforms automate evidence collection, access reviews and policy distribution. Thoropass states that subscriptions start at $99 per month for very small organizations and scale to enterprise tiers. Automation reduces staff time but still requires configuration and oversight.
- Prioritize high‑risk controls. Conducting a risk analysis early allows you to focus investments on controls that materially reduce risk rather than spreading budget evenly across all controls. A risk‑based approach ensures that funds address real vulnerabilities, not theoretical ones.
- Combine frameworks where possible. If you need HIPAA plus SOC 2 or HITRUST, plan audits together so evidence can be reused. Coordinated assessments may save 30–40% compared to separate engagements.
- Engage a managed compliance partner. Konfirmity differs from typical software platforms. We provide a human‑led managed service that implements security controls inside your stack and operates them continuously. With our support, organizations typically achieve SOC 2 readiness in 4–5 months compared with the 9–12 months common in self‑managed programs. Clients report a 75% reduction in internal effort and fewer audit findings because controls are designed and tested from day one.
Factors that influence cost
Several factors can increase or decrease your HIPAA Audit Cost:
- Size and complexity. More staff, more devices and more locations mean more policies, more logs and more points of failure. This drives up assessor time and remediation effort.
- Security maturity. Organizations with established cybersecurity frameworks (SOC 2, ISO 27001) often have many controls in place, so HIPAA readiness is less expensive. By contrast, those starting from scratch will need to build policies, processes and technical safeguards.
- Type and volume of PHI. Sensitive records such as mental health records or genetic data require stronger controls and can increase cost.
- Geographic and regulatory context. Labor costs vary by region, and some states impose additional privacy requirements that exceed federal HIPAA standards.
- Audit depth and frequency. Regular internal audits and continuous monitoring may seem expensive, but they often reduce the cost of external audits by catching issues early and providing up‑to‑date evidence.
Audit cost versus overall compliance cost
It’s important to distinguish between the price of an audit and the broader expense of complying with HIPAA. An audit is a snapshot validation. Compliance, by contrast, encompasses all administrative, technical and physical safeguards, ongoing risk management, workforce training, documentation upkeep, and vendor oversight. As noted earlier, the mid‑range estimate for achieving compliance in 2024 was $80,000–$120,000. By 2025, some guides estimated that full compliance programs could range from $25,000 to over $100,000 for smaller organizations and into the millions for large systems. When budgeting, view the audit as a line item within this larger program rather than assuming it covers everything.
Conclusion
Healthcare organizations have a duty to protect patient data. Ignoring security in the hope of avoiding audit costs is short‑sighted. Your size, scope, security maturity and technology posture influences the cost of a HIPAA audit. While fees and remediation expenses can appear high, they are small compared with the price of a breach or regulatory enforcement. Plan ahead, perform risk assessments, and invest in continuous monitoring. Your HIPAA Audit Cost should be viewed as part of a broader investment in security rather than a stand‑alone expense. By building a program that prioritizes real security outcomes and continuous evidence, you turn compliance into a natural by‑product of doing the right thing.
FAQs
1. How much does a HIPAA audit cost?
The cost depends on size and scope. Readiness assessments start around $5,000 for small organizations and can exceed $40,000. Auditor fees for formal assessments range from $15,000 to $200,000. Smaller clinics may spend under $20,000 in total, while large systems can exceed six figures when including remediation and technology upgrades.
2. Does HIPAA require an audit? \
HIPAA does not mandate routine certification. However, the Security Rule requires covered entities to conduct risk analyses and implement safeguards. OCR conducts audits and investigations to enforce compliance. Many organizations choose to undergo a third‑party audit proactively to identify and fix issues before OCR contacts them.
3. What is the cost of HIPAA compliance?
Achieving compliance involves more than an audit. Mid‑range estimates for full programs were $80,000–$120,000 in 2024. By 2025, some sources suggest that smaller organizations spend $25,000–$100,000, while large healthcare systems invest hundreds of thousands or millions. Costs include risk assessments, policy development, technology upgrades, training, and continuous monitoring.
4. Can a HIPAA fine be up to $50,000 for a violation?
Yes. OCR’s penalty structure includes a tier where willful neglect not corrected within 30 days incurs a minimum fine of $71,162 per violation. For criminal violations, fines can be $50,000 and higher. Civil penalties are capped at $2,134,831 per violation type each year. Budgeting for compliance reduces the chance of facing these penalties.





.svg)



.svg)
.svg)